Buntanetap is an oral molecule that selectively binds to an iron-responsive element in the mRNA of amyloid precursor protein (APP) and other neurotoxic proteins and inhibits their translation. Through this mechanism, buntanetap was shown to decrease the production of amyloid beta (Aβ), tau, alpha-Synuclein (αSYN), and TDP43.
Phase II/III Study
The Phase II/III study was a randomized, double-blind, placebo-controlled trial investigating the efficacy, safety, and tolerability of buntanetap in patients with mild to moderate AD. This was a dose-ranging study where patients received either one of three doses of buntanetap (7.5mg, 15mg, or 30mg) or placebo on top of their standard of care for 12 weeks. In this study, over 700 patients were screened, a total of 353 patients were enrolled, and 325 patients completed the study across 54 sites in the US. The study included mild to moderate AD patients whose Mini Mental State Examination (MMSE) scores at baseline ranged from 14 to 24. More information on the trial can be found on www.clinicaltrials.gov (NCT05686044).
Beyond safety, the trial assessed the changes in two co-primary endpoints: Alzheimer’s Disease Assessment Scale-Cognitive Subscale 11 (ADAS-Cog 11) and Alzheimer’s Disease Cooperative Study Clinician’s Global Impression of Change (ADCS-CGIC), which assess cognition and activities of daily living. The study monitored for safety and collected plasma to measure several biomarkers to assess the disease state, potential disease progression, and treatment effects.
ADAS-Cog 11 (Co-primary Endpoint) Shows a 3.3 Statistically Significant Improvement
We observed a significantly higher improvement in ADAS-Cog 11 scores in each treatment dose relative to placebo for patients with mild AD. The analysis focused on biomarker-positive early AD patients (MMSE 21-24, pTau217/tTau≥4.2%) found that ADAS-Cog 11 was highly statistically significant at all 3 dose levels and in the combined dose levels compared to placebo as well as to baseline (Figure 1). This objective measure of cognitive function confirms our findings from the two small Phase II studies that showed improvement in cognition in mild AD patients (Fang et al. JPAD 2023). The treatment response in the current study was not related to a patient’s age or sex.
Note 1: AD biomarker field has fast accelerated in the past few years. When we initiated the study in
Note 2: Our initial recruitment did not prescreen patients for AD biomarkers in plasma. When we became aware of issues from other AD studies with sites recruiting non-AD patients, we fast-tracked biomarker measurements by collaborating with
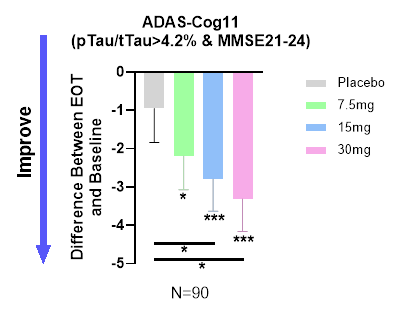
Figure 1. Dose-dependent improvement in cognition in the population with confirmed early AD.
At the end of 3 months of treatment, placebo group demonstrated slight improvement (LSM(SE), 0.26 (0.91)), but not significantly different from baseline. All three buntanetap treatment groups showed statistically significant improvement from their corresponding baseline (7.5mg improved 2.19 (0.87), p=0.013; 15mg improved 2.79 (0.81), p=0.001; 30mg improved 3.32 (0.82), P<0.001). Both 15mg and 30mg treatment groups also had a statistically significant improvement relative to placebo group (p=0.042 and 0.015 respectively). EOT- End of Treatment * P<0.05; ** P<0.01; ***P<0.001
Treatment Response is Highly Correlated to MMSE Score at Baseline
When we subdivided the baseline MMSE scores for patients positive for AD according to their pTau217/tTau >4.2% ratio, we observed a dose-dependent relationship to MMSE at baseline – the response to buntanetap treatment is more pronounced in mild AD patients than in those with more advanced AD. The response in the 30mg dose treatment group R2=0.17 (R² or the coefficient of determination), p<.001, indicates statistical significance of the MMSE score, which was not evident in the placebo group. Figure 2 confirms the efficacy of buntanetap as previously shown in Figure 1.
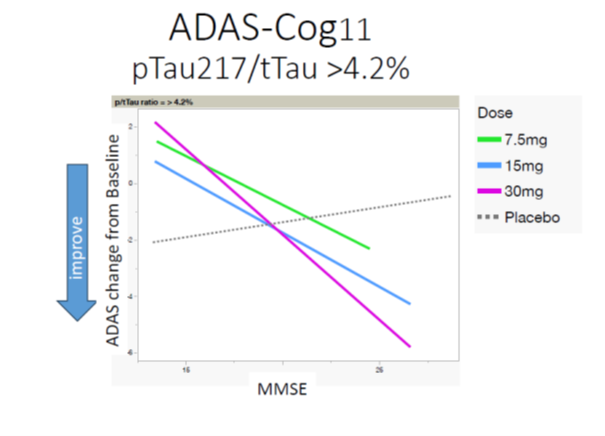
Figure 2. Buntanetap’s efficacy is strongly correlated with MMSE status.
Three-Fold Increase in Number of Responders in
A further look at responders versus non-responders showed a dose-dependent increase in the number of responders from placebo to 30mg. There was a three-fold difference in the proportion of participants who improved in the 30mg group relative to placebo (Table 1).
| Responders vs Non-Responders | |||
| Dose | Responders (Number & Percentage) | Non-Responders (Number & Percentage) | Total Number |
| Placebo | 6 (27.27%) | 16 (72.73%) | 22 |
| 7.5mg Buntanetap | 14 (73.68%)** | 5 (26.32%) | 19 |
| 15mg Buntanetap | 18 (72.00%) ** | 7 (28.00%) | 25 |
| 30mg Buntanetap | 21 (87.50%)*** | 3 (12.50%) | 24 |
**Contrast with Placebo, p value < 0.01, *** Contrast with Placebo, p value < 0.001
Table 1. Distribution of responders and non-responders in placebo and 3 doses of buntanetap.
Data presented in Figures 1, 2 and Table 1 demonstrate the efficacy of buntanetap in early AD patients.
Other Study Endpoints
ADCS-CGIC
This study was designed to enroll 80 patients per group with minor expectations for a statistically significant outcome in ADCS-CGIC or ADCS-ADL. We measured both endpoints to assess a possible trend that could support a power analysis for the sample size in the next disease-modifying 18-month study.
During the trial, ADCS-CGIC in all groups of patients barely changed, with no statistically significant difference observed. The 15mg and 30mg buntanetap groups slightly improved in mild AD patients. The subjective nature of this assessment allowed for a greater placebo effect, particularly in the advanced Alzheimer's population, as patients and caregivers were likely hopeful for change.
ADCS-ADL
We observed a large placebo effect in ADCS-ADL, with 15mg and 30mg buntanetap groups showing similar improvements with no statistical difference between the groups.
Biomarkers
In accordance with the mechanism of action of buntanetap, we observed a reduction in plasma tTau (total Tau) after treatment, providing further credence to buntanetap’s efficacy and mechanism of action (Figure 3).
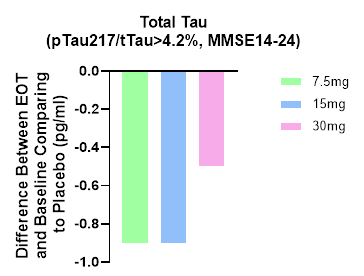
Figure 3. Total Tau levels are decreased at all 3 doses, which is consistent with our earlier Phase IIa data, where we also saw a decrease in tTau (Fang et al. JPAD 2023).
We plan to measure additional biomarkers for inflammation and axonal and synaptic functions.
Safety and Tolerability
Buntanetap was very well tolerated. The safety profile observed in this study was consistent with prior clinical trials, with comparable numbers of adverse events (AEs) between treatment and placebo groups. The majority of reported AEs were mild to moderate in severity. No serious AEs were related to buntanetap.
Summary
Next Steps
This short study shows a symptomatic effect with a possible disease-modification trend according to the tau data. The next study will have a longer duration, improved design and be statistically powered to validate symptomatic improvement and disease-modification.
Annovis will report the data to the FDA and ask for an end-of-Phase II meeting. We expect to discuss the data with the FDA in the next two to three months and then move on to the next Phase III study to confirm and expand these findings in an 18-month disease-modifying trial focusing on biomarker-positive early AD patients. We further plan to present the data at the AAIC2024 and to publish it in a peer-reviewed journal.
Kore Liow, MD, Director,
“These findings are a significant milestone for Alzheimer's patients. Buntanetap has the potential to be the first safe and convenient oral therapy that provides symptomatic efficacy while slowing disease progression. The mechanistic pathway and science are novel, and our physicians and researchers at the Hawaii Memory Center & Alzheimer's Research Unit are proud to have contributed to four studies and look forward to participating in future studies.”
“This Phase II/III Alzheimer study builds and expands on the understanding we collected in the Phase II studies. Based on buntanetap’s unique mechanism of action, we believe it can give patients both symptomatic and disease-modifying benefits. It’s really exciting to see that this study confirmed what we have observed in the previous Phase II studies in both the improvement of patients’ cognition and the improvement of biomarkers. We are unaware of any double-blind, placebo-controlled studies demonstrating this level of improvement in the ADAS-Cog 11 after one and after three months. We are preparing the data to discuss with the FDA on how to proceed to show disease-modification, for presentation at AAIC2024 and for publication.”
About Buntanetap
Buntanetap (formerly known as Posiphen or ANVS401) attacks neurodegeneration by inhibiting the formation of multiple neurotoxic proteins - amyloid beta, tau, alpha synuclein, and TDP43 - thereby improving synaptic transmission, axonal transport and neuroinflammation. Dysregulation of these pathways has been shown to be the cause of nerve cell degeneration and ultimately death. By attacking these pathways, buntanetap has the ability to reverse neurodegeneration in AD, PD, and other neurodegenerative diseases.
About
Headquartered in
Forward-Looking Statements
This press release contains "forward-looking" statements within the meaning of Section 27A of the Securities Act of 1933, as amended, and Section 21E of the Securities Exchange Act of 1934, as amended. All statements other than statements of historical fact are statements that could be deemed forward-looking statements. The Company advises caution in reliance on forward-looking statements. Forward-looking statements include, without limitation, the Company's plans related to clinical trials. These statements involve known and unknown risks, uncertainties and other factors that may cause actual results to differ materially from those implied by forward-looking statements, including regarding patient enrollment, the effectiveness of buntanetap and the timing, effectiveness, and anticipated results of the Company's clinical trials evaluating the efficacy, safety, and tolerability of buntanetap. See also additional risk factors set forth in the Company's periodic filings with the
Investor Contacts:
Maria Maccecchini, Ph.D.
maccecchini@annovisbio.com
References:
1. Fang C, Hernandez P, Liow K, Damiano E, Zetterberg H, Blennow K, Feng D, Chen M, Maccecchini M. Buntanetap, a Novel Translational Inhibitor of Multiple Neurotoxic Proteins, Proves to Be Safe and Promising in Both Alzheimer's and Parkinson's Patients. J Prev Alzheimer’s Dis. 2023;10(1):25-33. doi: 10.14283/jpad.2022.84. PMID: 36641607.
2. Ashton NJ, Brum WS, Di Molfetta G, et al. Diagnostic Accuracy of a Plasma Phosphorylated Tau 217 Immunoassay for Alzheimer Disease Pathology. JAMA Neurol. 2024;81(3):255–263. doi:10.1001/jamaneurol.2023.5319
3. Barthélemy, N.R., Salvadó, G., Schindler, S.E. et al. Highly accurate blood test for Alzheimer’s disease is similar or superior to clinical cerebrospinal fluid tests. Nat Med 30, 1085–1095 (2024). https://doi.org/10.1038/s41591-024-02869-z
4. Meyer MR, Kirmess KM, Eastwood S, et al. Clinical validation of the PrecivityAD2 blood test: A mass spectrometry-based test with algorithm combining %p-tau217 and Aβ42/40 ratio to identify presence of brain amyloid. Alzheimer's Dement. 2024; 1-14. https://doi.org/10.1002/alz.13764
Figures accompanying this announcement are available at:
https://www.globenewswire.com/NewsRoom/AttachmentNg/28dd23e3-bb6c-49e2-9522-4d4c894d934c
https://www.globenewswire.com/NewsRoom/AttachmentNg/5a4e081c-a8e3-46c1-8b76-e890aa18cd40
https://www.globenewswire.com/NewsRoom/AttachmentNg/da92d14a-c0b5-4ce9-8cdc-99830d75c078

Back to Top